

Resman F, Ristovski M, Forsgren A, Kaijser B, Kronvall G, Medstrand P, Melander E, Odenholt I, Riesbeck K. Invasive Haemophilus influenzae in British Columbia: non-Hib and non-typeable strains causing disease in children and adults.

Antibiotic susceptibility of invasive Haemophilus influenzae strains in Canada. dMH-F, Mueller-Hinton agar supplemented with defibrinated horse blood and β-NAD for susceptibility testing of fastidious organisms ( ). cOne beta-lactamase negative isolate from each laboratory, randomly selected from the isolates remaining after selection for the Resistant group. Information about the methodologies for susceptibility testing are included in the surveillance report.
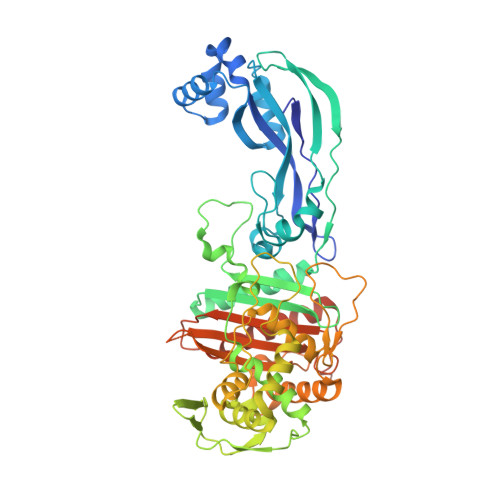
The selection criteria were constructed using epidemiological cut-off MIC values defined by EUCAST ( ) and zone diameter distributions from the surveillance report. The following selection criteria were used: amoxicillin-clavulanate MIC ≥2 mg/L, cefuroxime MIC ≥4 mg/L, cefotaxime MIC ≥0.12 mg/L and/or cefaclor 30 μg zone <17 mm (all isolates) and ampicillin MIC ≥1 mg/L, phenoxymethylpenicillin 10 μg zone <13 mm and/or ampicillin 2 μg zone <16 mm (beta-lactamase negative isolates). bAccording to phenotypic susceptibility profiles (by gradient MIC, disk diffusion and beta-lactamase detection) as reported by the primary laboratories. Flowchart showing selection and inclusion of bacterial isolates. Combining MLST and ftsI/PBP3 typing is a powerful tool for this purpose. The need of continuous monitoring of beta-lactam susceptibility and a global system for molecular surveillance of rPBP3 strains is underlined. The results indicate that horizontal gene transfer contributes to the emergence of rPBP3 by phylogeny restricted transformation.Clonally related virulent rPBP3 strains are widely disseminated and high-level resistant isolates emerge in new geographical regions, threatening current empiric antibiotic treatment. This study is the first to link ftsI alleles to STs in H. Several unrelated STs possessed identical copies of the ftsI allele encoding PBP3 type A.Infection sites, age groups, hospitalization rates and rPBP3 frequencies differed between STs and phylogenetic groups. The most prevalent substitution pattern (PBP3 type A) was present in 41% of rPBP3 isolates, mainly carried by ST367 and ST14. Group III high-rPBP3 was identified for the first time in Northern Europe.Four MLST sequence types (ST) with characteristic, highly diverging ftsI alleles accounted for 61% of the rPBP3 isolates. Group II low-rPBP3 predominated (96%), with significant proportions of isolates non-susceptible to cefotaxime (6%) and meropenem (20%). The prevalence of clinical PBP3-mediated resistance to ampicillin was 9%, compared to 2.5% three years earlier. The prevalence of rPBP3 in a population of 795 eye, ear and respiratory isolates (99% NTHi) from 2007 was 15%. We combined multilocus sequence typing (MLST) and ftsI/PBP3 typing to study the emergence and spread of rPBP3 in nontypeable H. Low-level resistant isolates with the N526K substitution (group II low-rPBP3) predominate in most geographical regions, while high-level resistant isolates with the additional S385T substitution (group III high-rPBP3) are common in Japan and South Korea.Knowledge about the molecular epidemiology of rPBP3 strains is limited. Beta-lactam resistance in Haemophilus influenzae due to ftsI mutations causing altered penicillin-binding protein 3 (PBP3) is increasing worldwide.


 0 kommentar(er)
0 kommentar(er)
